We study the fundamental mechanisms that regulate the formation and maintenance of the blood and lymphatic vascular systems in the body, and explore how these mechanisms are impaired in severe inflammation causing fluid leakage into tissues in various difficult-to-treat diseases.
Endothelial cells are key components of vascular systems, forming the inner lining of both blood and lymphatic vessels. The endothelial cells in our bodies form a semipermeable barrier estimated to cover an area comparable to that of six tennis courts. Malfunction or impaired integrity of the endothelial cell layer causes fluid accumulation in tissues. Fluid leakage from the blood circulation can impair blood perfusion and cause edema, which may lead to organ failure, for example in sepsis. However, stopping vessel leakage or improving lymphatic drainage remains a challenge in many diseases.
Comprehensive understanding of what causes vessel leakiness and how leaky vessels can be repaired, is incomplete. By studying the fundamental principles of how blood and lymphatic vessels are formed and how their stability is maintained, we aim to understand the mechanisms that cause vessel leakiness or malfunction in various human diseases. New understanding of mechanisms regulating vascular stability and proper functioning of lymphatic vessels facilitates translational research to improve vascular stability and function in various diseases.
Pathological vessel leakage
The blood and lymphatic vascular vessels regulate tissue homeostasis by controlling tissue fluid balance, inflammation and immune surveillance. The integrity of blood vessels is paramount for proper functioning of the vascular system. Impaired vascular integrity is associated with acute and chronic inflammation and pathological vessel growth in many common, but difficult-to-treat diseases, including cardiovascular, inflammatory, metabolic, and even neurological disorders (Nat Rev Drug Disc, 2017, review).
MOLECULAR REGULATION OF ENDOTHELIAL BARRIERS
Endothelial cells form organotypic vascular barriers and maintain vessel stability via coordinated signaling inputs by growth factors, cytokines and cell adhesive- and mechanical forces. Our group has discovered mechanisms of how the endothelial Angiopoietin (Angpt)-Tie growth factor receptor signaling pathway leads to vascular leakage (J Clin Invest, 2016). In addition, our group has discovered mechanisms by which Angpt-2 destabilizes endothelial monolayers via binding to beta1-integrin (PNAS, 2018). Moreover, we found that by inhibiting beta1-integrin using antibodies or deleting one allele of the Itgb1 gene in endothelial cells in mice, halted vascular leakage in a sepsis model and this improved cardiac function (PNAS, 2018). Mechanistically, we identified a novel cellular pathway regulated by the adapter protein Tensin1, which increased endothelial cell fibrillar adhesions and tension, leading to an increase in endothelial permeability (PNAS, 2018).
RESEARCH FOCUS
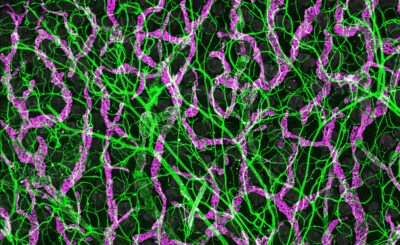
We use a multidisciplinary approach to uncover mechanisms of endothelial growth factor receptor pathways and integrins in regulation of vascular formation and maintenance. This includes inducible tissue type-specific gene deletions and various disease models, combined with imaging (confocal, light-sheet, intravital multiphoton microscopy and micro-computed tomography imaging), single-cell RNA sequencing and cell culture models, as well as biochemical, biophysical, and structural biology analyses (including protein crystallography and SAXS). We also collaborate with clinician scientists to elucidate pathophysiological mechanisms of vascular diseases.
Our main research areas include:
(1) Adhesive forces in vascular stability and permeability
(2) Mechanosensitive pathways in lymphangiogenesis and lymphatic vascular maintenance
(3) Molecular and atomic level understanding of adhesion receptor and growth factor receptor signalling crosstalk.
Mannion AJ, Zhao H, Zhang Y, von Wright Y, Bergman O, Björck HM, Saharinen P, Holmgren L. The junctional mechanosensor AmotL2 regulates YAP promotor accessibility. BioRxiv, doi: https://doi.org/10.1101/2023.01.13.523596
Tuohinto K, DiMaio TA, Kiss EA, Laakkonen P, Saharinen P, Karnezis T, Lagunoff M and Ojala PM. KSHV infection of endothelial precursor cells with lymphatic characteristics as a novel model for translational Kaposi’s sarcoma studies. In press, PlosPathogen
Korhonen EA, Murtomäki A, Jha SK, Anisimov A, Pink A, Zhang Y, Stritt S, Liaqat I, Stanczuk L, Alderfer L, Sun Z, Kapiainen E, Singh A, Sultan I, Lantta A, Leppänen VM, Eklund L, He Y, Augustin HG, Vaahtomeri K, Saharinen P, Mäkinen T, Alitalo K. Lymphangiogenesis requires Ang2/Tie/PI3K signaling for VEGFR3 cell-surface expression. J Clin Invest. 132:e155478. 2022
Characterization of ANGPT2 mutations associated with primary lymphedema. Leppänen VM, Pascal Brouillard P, Korhonen EA, Sipilä T, Jha SK, Revencu N, Labarque V, Fastré E, Schlögel M, Ravoet M, Singer A, Luzzatto C, Angelone D, Crichiutti G, D’Elia A, Kuurne J, Elamaa H, Koh GY, Saharinen P, Vikkula M and Alitalo K. 2020, Sci Transl Med. 12(560):eaax8013.
Targeting β1-integrin inhibits vascular leakage in endotoxemia. Hakanpaa L, Kiss EA, Jacquemet G, Miinalainen I, Lerche M, Guzmán C, Mervaala E, Eklund L, Ivaska J, Saharinen P. 2018, Proc Natl Acad Sci (U S A). 115:E6467-E6476.
Lymphatic endothelium stimulates melanoma metastasis and invasion via MMP14-dependent Notch3 and β1-integrin activation. Pekkonen P, Alve S, Balistreri G, Gramolelli S, Tatti-Bugaeva O, Paatero I, Niiranen O, Tuohinto K, Perälä N, Taiwo A, Zinovkina N, Repo P, Icay K, Ivaska J, Saharinen P, Hautaniemi S, Lehti K, Ojala PM. 2018, Elife 7. pii: e32490.
Tie1 controls angiopoietin function in vascular remodeling and inflammation. Korhonen E, Lampinen A, Giri H, Anisimov A, Kim M, Allen B, Fang S, D’Amico G, Sipila T, Lohela M, Strandin T, Vaheri, Ylä-Herttuala S, Koh GY, McDonald DM, #Alitalo K and # Saharinen P. 2016, J Clin Invest. 126: 3495-3510. *#equal
Endothelial destabilization by angiopoietin-2 via integrin 1 activation. Hakanpaa L, Sipila T, Leppanen VM, Gautam P, Nurmi H, Jacquemet G, Eklund L, Ivaska J, Alitalo K, Saharinen P. Nature Commun. 6:5962, 2015.
Current members
Elina A. Kiss, Postdoctoral Researcher
Anne Pink, Postdoctoral Researcher
Kumar Ponna, Academy of Finland Postdoctoral Researcher
Niina Santio, Visiting Researcher
Abhinandan Venkatesha Murthy, Postdoctoral Researcher
Keerthana Ganesh, Doctoral student
Tuomas Sipilä, Doctoral student
Ylva von Wright, Doctoral student
Aleksi Halme, Master’s student
Pihla Kaipainen, Master’s student
Heidi Toivonen, Master’s student
Konstantin Matjusinski, Undergraduate student
Shadi Jansouz, Laboratory coordinator
Former members
Seyedehshima Naddafi, Master’s student
Laura Seitakari, Med. student
Riina Lampela, Laboratory coordinator
Laura Hakanpää, completed PhD thesis in the group
Anita Lampinen, completed PhD thesis in the group
Eric Coles, completed M.Sc. thesis in the group
Prson Gautam, completed M.Sc. thesis in the group
Aleksi Halme, completed B.Sc. thesis in the group
Ciia Kohonen, completed B.Sc. thesis in the group
Ella Tuominen, completed B.Sc. thesis in the group
Noora Nurminen, completed B.Sc. thesis in the group
Lavinia van der Sande, Kaho Sint Leuven, Belgium, completed B.Sc. thesis in the group
Julie Drighe, Kaho Sint Leuven, Belgium, completed B.Sc. thesis in the group
Rita Teixeira, Ecola Superior de Saude, Porto, Portugal, Erasmus student
Joel Noutere, undergraduate student
Riina Haajanen, undergraduate student
Elisa Ritola, undergraduate student
Hanna Vihervaara, undergraduate student
Salla Välipakka, undergraduate student
Janina Allekotte, undergraduate student
Anni Ojansivu, undergraduate student
Seija Tillanen, Senior Laboratory Analyst
Kirsi Mänttäri, Laboratory technician
Janine Weis, M.Sc.